Undergraduate Policies
Undergraduate Policies
Purpose
The purpose of this policy is to outline the Accommodation and Access Policy specific to applicants and students of the College of Nursing and is in alignment with The Saskatchewan Human Rights Code and the University of Saskatchewan Policy: Duty to Accommodate This policy informs the procedures to be followed by College of Nursing faculty,* staff and students.
*Faculty includes Associate/Assistant Deans, faculty Resource persons, course coordinators, clinical associates, clinical instructors and lecturers.
Policy
The College of Nursing admits students who are academically qualified and have the potential to be successful in their program of study. The student population should reflect the diversity of Canadian society, including students with disabilities.
The Saskatchewan Human Rights Code requires the University of Saskatchewan to make reasonable efforts to accommodate a student with a disability, as recognized by Access and Equity Services (AES). For the purposes of this policy, the term disability is defined as such by the code.
The College of Nursing recognizes that students with disabilities may require accommodations. These accommodations provide students with disabilities the opportunity to participate in our programs. All students are required to meet program intents. Additionally, the professional regulatory body, the College of Registered Nurses of Saskatchewan (CRNS) outlines entry level competencies that must be met by graduates of the Bachelor of Science in Nursing (BSN): Registered Nurse Practice Standards (2019), and entry level competencies for graduates of the Master of Nursing - Primary Health Care Nurse Practitioner RN (NP) program (MN-NP) and Post-Graduate Nurse Practitioner Special Certificate (PGDSPC-NP) program: Nurse Practitioner Practice Standards (2017).
Purpose
To identify the process for the admission of students who have previously been required to discontinue (RTD) from the USask or other post-secondary institutions.
Policy
- Applicants must disclose all previous occurrences, including dates and length of RTD at time of application.
- Students are not considered for application during the 12 months of their RTD period.
- Students who have completed the required 12 month RTD period must provide a document that explains the reasons for the RTD and demonstrates a plan for future success.
- Students who have been RTD twice may be considered in exceptional circumstances.
- Students who are admitted to the College of Nursing after completing their RTD period must repeat all BSN courses that they received below 60%.
Purpose
The purpose of this policy is to establish the expectation of student attendance for all orientations, classes, seminars, labs, and clinical experiences throughout their program of study.
Policy
- Attendance at all orientations is mandatory and cannot be missed. Exceptions may be considered for unavoidable circumstances (e.g., illness, bereavement). Students must contact the course lead in these situations to discuss potential for alternate arrangements.
- Regular and punctual attendance is expected of all students for all orientations, classes, seminars, labs, and clinical experiences. A student who is consistently late and/or absent from classes, seminars, and/or labs may be unable to meet the course requirements and may not be able to receive credit for the course. If a student misses more than 10% of clinical/lab experiences in a course with faculty led clinical/lab groups, they will require a discussion with the course coordinator and may be unable to meet the course requirements.
- Students in preceptored clinical placements are expected to complete all clinical hours to obtain credit for the course.
- If a student is unable to attend or will be late for a lab or clinical experience, they must notify the instructor prior to the start of the learning experience.
- Attendance at classes, labs, and/or seminars for the particular course may be designated as mandatory. Students must attend these learning experiences in order to receive a pass in the course.
- If an instructor deems a student unsafe or unprepared for a learning experience, the student may be excluded from the experience; thus, the student may not be able to meet the course requirements.
Purpose
To set expectations and guidelines for the use of cellular phones in classroom and lab.
Policy
The use of cellular phones in classroom, lab and clinical settings must be respectful and must not interfere with the learning experience of the owner or those around them. In clinical settings students are expected to follow the mobile device usage policy.
- Many courses in nursing will require the use of a smart phone for academic, research and point of care purposes. Students are expected to bring these devices to class with them when required.
- Audible feedback from the device (including ringtones, vibrations and keystroke chimes) should be silent to minimize disruption to others.
- Personal use of cell phones and texting should be kept to a minimum in classroom and labs.
- In clinical setting, students and instructors are expected to follow agency policy and are expected to follow the mobile device usage policy.
Purpose
To delineate the process for completion of course requirements.
Policy
- Students are required to complete all course components to receive credit for a course.
- Unless prior arrangements have been made with the course instructor, 5% from the earned grade for that assignment will be deducted for each calendar day that course work is late. A grade of zero will be applied to all assignments not submitted 5 working days after the due date, without prior written permission of the course instructor.
- Unless other arrangements have been made with the course facilitator, the last day for acceptance of assignment will be the final day of class in that course.
- It should be noted that even if assignments receive a grade of 0% because of late penalties (see above), they must still be completed in order to fulfill course requirements.
Purpose
To provide students in the College of Nursing with guidelines for maintaining patient confidentiality.
Policy
- Because students, by virtue of being such, have access to and are allowed to collect confidential information about persons or institutions or their representatives for the purposes of doing studies and writing papers, it is necessary to have some limitation on the distribution of material. This material should be restricted to the teacher and those preparing the paper.
- If material is suitable for publication, permission to publish must be obtained from the teacher concerned, as well as the Dean of the College.
- In order to maintain confidentiality, persons are not to be identified in any required written work of a course or on any permanent verbal record unless written permission of the person(s) involved is first obtained. Please refer to Student Confidentiality Agreement.
- Policies of any agency or institution concerning confidentiality are to be respected in a similar manner.
Purpose
To ensure CPR requirements are clear and consistent for all undergraduate students.
Policy
- Students must provide evidence of current CPR certification prior to the start of the first clinical experience and must maintain current CPR certification, throughout the program. Current CPR/expiry is defined by the organization providing the certification.
Note: The certification must include theory AND hands on skills training for choking, CPR, and AED for infant, child, and adult.
- Students failing to provide evidence of current CPR certification will be excluded from clinical practice.
Purpose
Health care workers are in a position of public trust and as such, are required to have a criminal record check with a vulnerable sector search for employment in health care settings. This policy is to ensure that nursing students meet that same requirement, and are therefore eligible for all clinical placement opportunities during the program.
Policy
- Nursing students accepted for admission into the College of Nursing programs are required to provide the results of a criminal record check, including a vulnerable sector search, after admission.
- Students failing to provide the results of a criminal records check will not be allowed to participate in any clinical experience requiring client care.
- Criminal record checks may be required to be forwarded to the health authority or agency upon their request.
- Additional criminal record checks may be required by specific clinical agencies as a condition of placement. Failure to provide such information will result in the agency excluding the students from clinical experience.
- Any costs associated with the criminal record check will be the responsibility of the student.
- Students are required to report criminal convictions and/or outstanding charges that occur after the date of the original criminal record check to the Associate/Assistant Dean of their site/program. Failure to report any criminal convictions and/or outstanding charges will be grounds for immediate dismissal from the program.
- Each reported criminal conviction and/or outstanding charge will be assessed to determine what, if any, impact the criminal conviction and/or outstanding charge will have on the student’s status in the program.
- In the event of a positive criminal record check, the Associate/Assistant Dean is required to forward this information to the health authority/agency representative, to determine eligibility of the student for clinical placements. The student may be required to provide the health authority with more information regarding the conviction.
- Access to criminal record check information, within the College of Nursing, will be limited to the Associate Dean/Assistant Dean, clinical coordinator(s) and the administrative support person for the clinical coordinators.
- A copy of and/or the original criminal record check will be on kept on file in a secure location, by the program for the duration of the students program.
- All student information regarding criminal record checks will be destroyed within 2 months after the student has completed the program or permanently withdrawn.
- Current and potential students with criminal records may be counseled to seek a pardon.
Purpose
To define the process for the exemption of final examinations at the College of Nursing.
Policy
- The Undergraduate Education Committee will approve all courses exempt from the University of Saskatchewan final examinations schedule.
- Applications for approval of exemption can be submitted to the chair of the Undergraduate Education Committee.
- The Associate Dean will provide the Registrar with a list of all courses that are exempt from the University of Saskatchewan final examination schedule.
Purpose
To delineate the process for grade assignment in the BSN/PDBSN.
Policy
- A student will be assigned the grade earned unless otherwise specified.
- Some nursing courses have an essential component that must be passed in order to pass the course. A student that has failed an essential component of a course, as defined in a course syllabus, will not be eligible to write the final exam and will not receive credit for the course. In the event that the essential component is failed, but the computed final grade results in a passing mark, an N (No credit) grade will be added to the computed percentile grade. A course with an N Grade assigned must be successfully repeated for the student to progress in the BSN program.
- A student that has not completed an essential component of a course, as defined in a course syllabus, will not be eligible to write the final exam and will not receive credit for the course. In the event that the essential component is not completed, but the computed final grade results in a passing mark, a final grade of 49% will be submitted along with a grade comment of an INF (Incomplete Failure).
- If a student has completed a course that is required but is given an N or an INF grade it will count towards the weighted average until it is successfully completed.
- Some clinical courses have an essential component, as specified in the course syllabus that must be successfully completed to continue in the clinical experience. When such an essential component is failed the student will not be allowed to continue in the clinical experience. The student can withdraw at this time. In the event that the withdraw deadline date has passed, the student will be given the grade earned.
- Students who withdraw from a class will not be eligible to submit an academic appeal.
- In courses that have multiple clinical components, a student must pass each clinical component in order to pass the course.
- A minimal pass grade of 50 - 59, as per the Literal Descriptors, in clinical is only allowed once throughout the program. If a student obtains a minimal pass a second time, the student will receive an N (No credit) grade and will be required to repeat the course and receive a minimum of a satisfactory grade of 60 - 69, as per the Literal Descriptors, in that clinical course and in all subsequent clinical courses.
Purpose
This policy is to ensure that students' hand hygiene during practice education placements in the RHAs/SCA meet infection control standards.
Hand Hygiene means any method that removes or destroys microorganisms on hands.
Policy
- Students will consistently perform proper hand washing techniques during clinical placements as defined by the current best standards and practices used in the clinical placement.
- Proper hand hygiene will be taught by the College of Nursing in the appropriate lab course/setting utilizing current best standards as defined by Infection Prevention and Control Canada.
- Students will follow the current hand hygiene policy and procedure of the agency during each of their clinical placements.
- Students deemed to be in violation of this policy will be required to review this policy and proper hand hygiene techniques with their instructor. Students found to be in repeated violation of this policy may be asked to leave their placement. It will be up to the RHA/SCA to determine if the student can return to the facility. In this case, the time away will be considered under the Attendance Policy.
Purpose
To establish consistent recommendations for student immunization. Immunizations help protect the health and safety of patients /clients, as well as nursing students participating in clinical placements.
Policy
- All nursing students are required to complete the recommended immunizations for health care workers as outlined in the most current Saskatchewan Immunization Manual (SIM) (Chapter 7, Section 6.5 Publicly Funded Vaccines - Healthcare - RHA/SCA/CC/FNJ and Students) prior to any contact between students and patients/clients.
- Students are required to submit to the College of Nursing proof of immunizations prior to participation in clinical experience.
- Students who do not complete recommended immunizations or required titre testing will be excluded from certain clinical areas as determined by the RHA/SCA. Therefore failure to maintain recommended immunizations may delay a student's progress in his/her studies.
- Students who do not complete recommended immunization(s) must sign a waiver and may be excluded from some clinical areas. The student may be at risk of not being able to complete required components of their program.
- Additional immunizations may be required for certain clinical placements and in specific circumstances, such as disease outbreaks. Students who refuse or are unable to comply with this requirement may be at risk of not being able to complete required components of their program.
- Students are to follow the RHA/SCA policy regarding influenza vaccination.
- In the event of influenza or other outbreak, any unvaccinated or non-immune student will be excluded from the outbreak area and will not be allowed to return until the RHA/SCA has determined it is safe to do so (i.e. infection, prevention and control; occupational health and safety). In this case, the time away will be considered under the Attendance Policy.
- Students who are applying for international clinical experiences will be required to meet the immunization requirements for the destination country.
- Any applicable costs of immunization are the responsibility of the student.
- Students must inform their on-site faculty and/or site supervisor of immunization status in relevant clinical situations.
- Students will inform their on-site faculty and/or site supervisor of onset of symptoms of a vaccine preventable communicable disease or contagious infection and exclude themselves from clinical placement as appropriate.
Purpose
To outline guidelines regarding the completion of midterm examinations in the College of Nursing.
Policy
- A student who is absent from a midterm examination through no fault of his or her own, for medical, compassionate, or other valid reasons, may contact the faculty member for the course in which they are registered for a deferred exam. Such application must be made within three business days of the missed examination and be accompanied by supporting documentary evidence.
- Faculty and/or the College of Nursing will not accommodate a request to reschedule a midterm exam because of personal reasons. Midterm examinations can be scheduled at any time during the academic term. Students should avoid making prior travel arrangements or other commitments that may conflict with scheduled exams.
- Missing a midterm examination due to personal or travel related conflicts may result in a midterm exam grade of 0% being assigned.
- In some exceptional circumstances, faculty may consider combining the weight of the missed midterm exam with the final exam. Students need to speak with the specific course faculty member prior to the missed midterm examination for this consideration.
- If the midterm and final exam are combined and the resulting weight of these components exceeds 50% of the final grade, approval must be sought from the Chair of the Undergraduate Education Committee.
Purpose
The purpose of this policy is to balance the learning needs of College of Nursing students with the risks of allowing them to access PHI (Personal Health Information) and health authority information using mobile devices and computers. The policy will establish standards, responsibilities and restrictions for College of Nursing students when using mobile devices in clinical environments.
Policy
- Students will not use personal devices to access PHI in RHA/SCA data systems unless pre-authorized by their education programs and the Information Technology (IT) department within the RHA/SCA in which they will be accessing information and data systems.
- Students can use personal or RHA/SCA provided mobile devices in clinical areas to research health information on the internet or connect to course required apps for purposes of providing health services to patients or for learning needs or course requirements specific to their placement learning objectives. Use of mobile devices for personal reasons should be conducted away from clinical areas and should be limited to break times except in emergencies. Use of mobile devices in clinical areas should never interfere with patient care or negatively impact the perception of services being offered to the patient. Whenever possible students should have their personal phones set to silent or vibrate unless they are required to be available to a supervisor.
- Students are never permitted to use non-RHA/SCA email accounts for communicating PHI. Communication via email of PHI may only be done between two email accounts from the same organization; inter-RHA/SCA emailing of PHI is not permitted.
- Mobile devices provided by the health authority to a student will be subject to all policies of the RHA/SCA related to mobile devices including password protection, internet acceptable use and privacy and confidentiality.
- Students that are granted remote access to RHA/SCA information systems from a personal device for patient care or course requirements must abide by the RHA/SCA policies and procedures regarding access to information systems including policies and procedures on remote access to information systems and password protection. Personal devices used in this manner must also employ any security measures deemed necessary by the RHA's/SCA's IT department. RHAs/SCA may require students to complete an application form to be granted remote access on personal devices.
- Students shall never make modifications, disable or tamper with RHA/SCA owned and installed hardware or software configurations. This includes, but is not limited to: data encryption, screen-saver passwords and anti-virus software.
- Students shall never install any software on RHA/SCA mobile devices without prior authorization.
- Students shall never permanently store information from a RHA/SCA information system or PHI (including photos, video or audio recordings, or text messages) on a mobile device or removable media. This information must be saved as appropriate to the RHA/SCA network or information system (or otherwise added to the patient's chart or record of care) and permanently removed from the mobile device or media as soon as possible. Saved images must follow the consent policies and procedures of the RHA/SCA.
- Students will not take photos, videos or audio recordings of patients, including close up pictures of wound, rashes, etc. except in exceptional circumstances when required by their supervisor for the immediate care of a patient. Photographs and PHI cannot be shared through an unsecure network (e.g. texting).
- PHI (e.g. text, photos, videos, or audio recordings) may only be communicated between mobile devices via texting if students utilize a secure, RHA/SCA-hosted messaging service (i.e. messages in transit are encrypted; photos taken are taken within an app and not inadvertently accessible, shared, or synced with the phone's default photo library or cloud; and the RHA/SCA hosts/controls the messaging server). If in doubt, students shall consult their RHA/SCA IT department and Privacy Officer.
- An insecure medium (e.g. texting, emails other than between two email addresses from the same RHA/SCA) may only be used to communicate PHI (text, photos, videos, or audio recordings) in the following circumstances:
- The patient or legal guardian has provided informed written or verbal consent (he/she must have had the risks explained to them), or
- It is an emergency situation where the benefit to patient outweighs the risks.
- Students will not take pictures of other students or staff in the clinical setting or pictures of the clinical setting itself unless permission has been obtained from the clinical supervisor and from those in the picture. Photographs taken must not include any patients (including in the background).
- All touch surfaces of IT devices used at, or near, point of care must be cleaned and disinfected (per manufacturer's instructions) with a hospital-grade disinfectant if used or touched during the encounter with the patient.
- Students using their own device or assigned a device from the RHA/SCA are responsible for routine cleaning and disinfection of the device.
- Devices that cannot be adequately cleaned and disinfected should not be used during placements.
- Students will employ expected physical security measures for any mobile device or removable media used for RHA/SCA business, especially when they contain RHA/SCA data. This applies whether or not the devices are actually in use and/or being carried. This includes, but is not limited to passwords, encryption, and physical control of such devices (e.g. securing laptops at workstations or in offices with a cable lock).
- Immediately report lost or stolen mobile devices or removable media to their Manager and/or as required by their respective RHA/SCA policy and procedures.
- Return RHA/SCA mobile devices to a manager/director/supervisor or designate when no longer needed or when the clinical placement is complete. Non-RHA/SCA devices that no longer require access to a RHA's/SCA's network, applications or data must be wiped clean of all information related to the clinical experience including information regarding RHA/SCA information systems and PHI and/or reset to factory settings. If uncertain on how to do this, contact the RHA's/SCA's IT department for assistance.
- Non-compliance with this policy will result in a review of the incident by the RHA/SCA and the educational institution. A review of non-compliance may result in:
- Temporary or permanent loss of privileges for access to some or all computing and networking resources and facilities.
- Disciplinary action by the manager, up to and including termination of the placement by the RHA/SCA or educational institution.
- Legal action according to applicable federal and provincial laws and contractual agreements.
Definitions:
App means an application that is typically a small specialized program downloaded to a mobile device.
Mobile Device means a laptop computer or a pocket-sized computing device (a device typically having a display screen with touch input or a miniature keyboard that can store electronic data files and software). A mobile device includes but is not limited to: laptop computer, tablet computer, personal digital assistant (PDA), cellular phone, smart phone, smartwatch, and ultra-mobile PC (UMPC). This includes home PCs and personal mobile devices used to access RHA/SCA's network, data, or applications.
Patients are the recipient of health care services or consultations provided by the RHA/SCA. This term includes clients and long-term care residents.
Personal Health Information (PHI) means, with respect to an individual, whether living or deceased:
i. information with respect to the physical or mental health of an individual;
ii. information with respect to any health service provided to an individual;
iii. information with respect to the donation by the individual of any body part or any bodily substance of the individual or information derived from the testing or examination of a body part or bodily substance of the individual;
iv. information that is collected: (A) in the course of providing health services to the individual; or (B) incidentally to the provision of health services to the individual; or
v. registration information;
vi. images including photographs
Regional Health Authorities (RHAs), as defined by The Regional Health Services Act, provide most health services in Saskatchewan, either directly or through affiliated health care organizations.
Remote Access means communication with a health authority information system or network using a mobile device from a remote location or facility through a public-accessible data link (e.g. Internet or modem). Some of the more common methods of providing this type of remote access are: remote dial-in through a modem, virtual desktop, login through the Internet (with programs or apps such as Citrix), Outlook Web access and remote email/calendar synchronization via the cellular network.
Removable Media means storage media that can store electronic data files or software and be removed from its device reader. Removable media includes, but is not limited to: memory cards, USB flash drives, pens that digitally record data, CDROMs, DVDs, or data backup or storage tapes.
RHA/SCA information system refers to any system that captures, stores, manages or transmits information related to the health of individuals or the activities of organizations that work within the health sector.
Saskatchewan Cancer Agency (SCA) is responsible for the planning, organization, delivery and evaluation of cancer care and related health services throughout the province.
Unsecure Network means a wireless network that you can access without entering a password. Wireless connections available in cafes or from creating a local "hotspot" with a personal phone are examples of unsecure networks.
Purpose
This policy provides guidance in the preparation, administration and recording of narcotics by undergraduate nursing students.
Policy
- Access to narcotics through automated dispensing systems will be defined by the individual agency.
- 2nd & 3rd year students: Preparation and administration of a narcotic must be directly supervised and co-signed by the clinical instructor.
- 4th year students: Removal and preparation of all narcotics must be directly supervised by the preceptor/designee.
- In the event that there is narcotic wastage students are not allowed to be the witness for wastage. They may however be a third signatory if they are directly involved in the administration of the narcotic.
- If the student signs for the count, it must be co-signed by two other registered staff. The student may not carry the narcotic keys. Students working with an RN are required to ensure ongoing accuracy of narcotics counts. Discrepancies in the narcotic count must be resolved upon discovery.
- Students may not pick up or accept narcotics from the Pharmacy.
- Students may monitor, record, and discontinue a PCA pump under the direct supervision of the clinical instructor/preceptor, and may care for a client with this equipment. Students may not start or adjust the PCA Pump.
- Students must follow the medication administration policies of the agency at all times.
* We wish to specifically acknowledge and thank the University of Windsor for the work they have done and shared with the College of Nursing, University of Saskatchewan.
Purpose
Considering the role of the College of Nursing in mentoring professional nursing students in a direct patient care role, the purpose of the policy is to assist with the identification and management of Patient Safety Incidents (formerly referred to as adverse events, sentinel event, near miss, close call, no harm incident and critical incidents), and to minimize risks and potential injuries to patients/clients/residents and students. College of Nursing Incident Management includes actions and processes required at the College level to conduct the immediate and ongoing activities following an incident. Part of incident management, Incident Analysis is a structured process that aims to identify what happened, how and why it happened, what can be done to reduce the risk of recurrence and make care safer, and what was learned (CIACP, 2012). This policy details actions to be taken by College of Nursing students and faculty upon recognition of a Patient Safety Incident.
Policy
- Patient Safety Report. Patient Safety Incidents are to be reported in a timely manner as soon after the event as possible. The College of Nursing Patient Safety Report Form should be completed by either faculty members and/or students and submitted to the course coordinator. Local health region incident report forms should be completed and submitted as required by health region policy. The Patient Safety Report Form shall be revised as needed to support College processes according to this policy.
- Immediate Action. In the event of a Patient Safety Incident the student is to follow the Health Region Policy and Procedures. Upon receipt of a Patient Safety Report Form, the clinical instructor and course coordinator shall ensure that immediate action is taken to care for and support patient/family/providers/others, secure items, and reduce risk of imminent recurrence.
- Discipline and fear of reprisal. The success of the Patient Safety Incident policy relies on the creation of a confidential environment where participants can safely report incidents and express their opinions about underlying contributing factors without fear of reprisal. The clinical instructor and course coordinator, in consultation with the Associate Dean as needed, shall determine whether the Patient Safety Incident is a result of actions of intention, recklessness or of unforeseen circumstance or complications of care, and such determination shall guide disciplinary action or impact on student grades or progress in the program. In general, faculty response to Patient Safety Incidents should facilitate student learning and be aligned with the educational mission of the College.
- Preliminary Investigation. The course coordinator shall report and forward a copy of the Patient Safety Report Form to the site’s Associate Dean. A College of Nursing Patient Safety Committee shall be responsible for reviewing incidents.
Upon receipt of the Patient Safety Report Form, a preliminary investigation of the incident shall ensue to understand what happened, how and why it happened, and to develop and manage recommended actions. Patient Safety Incident analysis involves systems thinking using a non-linear approach that includes consideration of categories of contributing factors (task, equipment, work environment, patient, healthcare team and organization factors) and use of multiple sources of information.
- Report. Recommendations shall be developed after each Patient Safety Incident addressing how to reduce risk of recurrence and make care safer, how student/faculty learning can be facilitated to prevent such an incident in future, and to determine what was learned and how learning should be shared. A formal report of the committee shall include recommended actions, implementation plan and monitor and assess the effectiveness of actions.
- Disclosure. The course coordinator shall collaborate with local health region to begin disclosure process, which should explain to patient/residents/family the unexpected event or change; offer an apology that it happened; assist patients/residents/families to understand how and why it happened; explain what will happen next and commit to next steps; and include patients/residents/family in the fact gathering process, enabling them to contribute what is known from their perspective (CIACP, 2012). The College Patient Safety Committee shall share what was learned internally (at minimum with the course coordinator and year committee) and externally (at minimum with the agency where the incident occurred). Sharing with external agencies shall occur in face to face meetings or in writing, and is the responsibility of the leadership team or designate. Sharing activities shall maintain patient/client/resident and student confidentiality.
- Aggregate Review. College Patient Safety Committee shall review annually all Patient Safety Incidents submitted to the College of Nursing from all sites. The goal of aggregate review is to ensure that patterns of incidents can be assessed, if present, and identify needed changes to College processes and curriculum to minimize risks and potential injuries to patients/clients/residents, students and faculty.
References
The framework was developed collaboratively by the Canadian Patient Safety Institute (CPSI - now Healthcare Excellence Canada), the Institute for Safe Medication Practices Canada, Saskatchewan Health, Patients for Patient Safety Canada, Paula Beard, Carolyn Hoffman and Micheline Ste-Marie. The framework is based on the 2006 Canadian Root Cause Analysis Framework.
https://www.healthcareexcellence.ca/media/gilnw3uy/canadian-incident-analysis-framework-final-ua.pdf
Purpose
To define how grades are released to students in the College of Nursing.
Policy
- Student grades achieved throughout a course (with the exception of the final grade in a course) will be posted on Canvas, as per course guidelines. Such grades will only be accessible by individual students once they have signed into their Canvas course, thereby protecting student confidentiality.
- Final grades assigned to students upon completion of a course will not be posted on Canvas courses. Students will only be able to access their final grades through PAWS.
Purpose
The purpose of this policy is to outline the processes to be used by instructors and students when students demonstrate unsafe or potentially unsafe performance in the clinical or lab setting.
Underlying principle:
The student and the program have a joint responsibility for facilitating student success in providing safe and competent nursing care.
These processes are predicated by the following standards of evaluation:
Clear direction of performance expectations, course intents, policies and evaluation processes, which have been provided to the student during orientation; provision of the opportunity for growth; timely feedback (verbal and/or written).
In a situation where a student's performance places the client, instructor/preceptor, or staff at a foreseeable risk, the student may be dismissed immediately from the clinical site. Dismissal from the clinical site is not indicative of clinical failure.
Definition of Unsafe Practice
From the literature: "Unsafe clinical practice is behaviour that places the client or staff in either physical or emotional jeopardy. Physical jeopardy is the risk of causing physical harm. Emotional jeopardy means that the student creates an environment of anxiety or distress which puts the client or family at risk for emotional or psychological harm. Unsafe clinical practice is an occurrence or pattern of behaviour involving unacceptable risk" (Scanlan, Care & Gessler, 2001). Dealing with the unsafe student in clinical practice. Nurse Educator, 26[1], 23-27). According to Killam, Luhanga, & Bakker (2011) unsafe practice includes any action, attitude or behaviour related to:
- ineffective interpersonal interactions, including communication and relational difficulties
- knowledge and skill incompetence, including deficits or failures of appropriate application
- projections or reflections of an unprofessional nursing image.
From University of Saskatchewan College of Nursing faculty and student focus groups: Unsafe practice is any practice that poses an actual or potential threat to the health of a client, including physical, psychosocial, or cultural safety. Unsafe practice includes harm not only to client, but also to colleagues or oneself.
The recent literature on patient safety identifies that a number of factors can come together to create an error. Therefore, an individual may be involved, but may not be solely responsible. When examining a situation(s) deemed as involving unsafe practice, it may be useful to examine it in terms of "what happened?", "why did it happen?" and "what could be done to prevent it from happening again?”.
A strong emphasis on patient safety is essential in nursing education to inform future nurses and increase patient safety (CASN & CPSI, 2018). As a profession, nursing faces significant challenges in terms of creating and maintaining a safe practice environment. The Canadian Nursing Association in their Nurses and Patient Safety discussion paper (CNA, 2004) identified that additional challenges to safe nursing care include: Nursing practice environment and workforce issues, team work and communication, nursing perspective on patient safety, and the patient perspective on patient safety, technology and culture of blame. Students who are learning to be nurses are learning to adapt to working within the present health care system, and therefore may also be affected by some of the additional systemic factors that impact patient safety. In the interest of creating and maintaining safe practice environments for patients and nurses, students must meet the standards of safe practice.
The following themes and behaviors were synthesized from the focus group feedback.
Behaviors that may be indicators of unsafe practice:
It should be noted that students and faculty identified the importance of context and patterns in relation to unsafe clinical performance. These behaviours are examples and are not meant to be inclusive of all behaviours.
- Lack of accountability, unprofessional practice:
- does not accept responsibility for own actions, does not admit mistakes, covers up errors is dishonest
- does not recognize potential for doing harm, lack of insight is reluctant to assume a professional role
- does not make the effort to learn, is not interested breaks confidentiality
- does not ask for help when unsure
- demonstrates inappropriate boundaries.
- Patterns of behavior:
- demonstrates a pattern of problems in clinical areas disregards policy
- does not know policies
- is frequently late or absent
- does not change behaviour in response to feedback; repeats mistakes even after feedback.
- Unmet competencies:
- has a poor knowledge base
- is unable to apply concepts and theory in practice
- poor and/or inconsistent skills in assessment and client care
- unable to set priorities; unable to care for clients at level of complexity expected for the course.
- Inconsistent communication and lack of respect:
- lack of respect for clients, aggressive with clients
- ineffective communications with client and staff.
- Lack of judgment:
- poor clinical judgment
- goes beyond own scope of practice
- evidence of impaired judgment due to drugs, alcohol, or lack of sleep
- demonstrates extreme anxiety that is disproportionate to the situation.
Sources of information when identifying students who may be practicing unsafely:
- For instructors/faculty:
- direct observation and supervision
- information from patients, families, staff members, other students, intuition - unable to trust student
- student care plans, charting and journals poor performance in previous rotations student avoids instructor
- critical incidents such as medication errors, client injury.
- Feedback from students regarding what they think they should do if another student is practicing unsafely:
- a student who is practicing unsafely is responsible to admit his/her own mistakes
- it is important, as a peer, to provide feedback when one sees another student practicing unsafely. Ask the student if he/she needs help
- if reporting the behaviours to the instructor, do so privately and not in front of the rest of the group
- do not help the student cover up by doing his/her work or always checking to see if he/she has done what needs to be done.
Suggestions for risk management in relation to students who may be practicing unsafely:
- Clinical instructors or the Faculty Resource Person (FRP), in consultation with preceptors, should keep anecdotal notes on all students and encourage students to keep their own notes about clinical situations.
- Where possible, equally distribute students requiring additional support among clinical groups.
- Where possible, the instructor should adjust assignments so client safety is not compromised, while still maintaining student ability to meet course intents.
- During orientation to the course outline the policy and processes for students who demonstrate unsafe practice. Clinical instructors/FRP should discuss during orientation and/or post conference explicit expectations for the clinical area with respect to safe practice (e.g. highlight areas where mistakes are commonly made and discuss strategies for prevention).
- Have another instructor help with assessment/evaluation of student performance.
- Associate/Assistant Dean may be asked to review patterns of performance from other clinical courses.
Suggestions for fairness to the student in the process of helping him/her practice safely:
- Discuss with student in private, try to identify cause of the problem, level of insight and self-awareness. Give the student a chance to explain.
- Acknowledge level of student and clinical expectations at that level. Don't compare one student with another.
- Provide timely feedback.
- Set out an action plan with student and identify specific criteria that must be met. Validate information that comes from another student and/or staff.
Section A: Processes to be used when there is unsafe practice in the clinical/lab setting.
1. Unsafe performance issue identified:The clinical instructor or FRP, in consultation with the preceptor, will document all aspects of performance (may include anecdotal notes, descriptive narrative, discussions with health personnel, examples of student charting, and/or written plan of care). A summary of the unsafe practice issues will be included in the course clinical evaluation. Instructor will discuss performance issues with the student and follow up with written documentation of the discussion sent to the student’s PAWS email account and cc course coordinator. The student must reply stating they have read and received feedback regarding the performance issues prior to returning to the clinical setting (if eligible).
Performance issues may be resolved at this juncture or may move to Process #2 or directly to Section B.
2. Severity of issues, additional issues, and/or continued pattern of issues previously identified that put the student at risk of failing or student receives minimal pass grade:The student will be placed on a Student Learning Plan (SLP) prior to continuing in the clinical setting. The SLP will outline performance issues and identify the standards and competencies at risk of not being met. The SLP will clearly outline the skills, behaviours and attitudes to be demonstrated by the student within a specified time frame, including the consequences of not meeting the terms of the SLP.
The SLP will be reviewed with the student in a meeting with the Clinical Instructor/FRP and/or Course Coordinator. An Academic Advisor and student support persons may be present. The student will be encouraged to meet with an Academic Advisor. A copy of the SLP will be sent to the student’s PAWS email account (cc clinical instructor/FRP and Course Coordinator; cc advisor if indicated) and the student must reply stating they have read and understood the SLP prior to returning to the clinical setting (if applicable).
The SLP must remain in place until the student has had an opportunity to demonstrate a satisfactory performance in the at risk competencies. If the clinical rotation does not provide the opportunity to evaluate student’s performance relative to the at risk competencies (e.g. management and organization of care for multiple patients cannot be evaluated in settings with a 1:1 RN patient ratio; giving multiple medications by various routes cannot be evaluated in settings with limited medication administration opportunities, lack of time in rotation after initiation of contract) the contract must be carried forward to the next clinical rotation.
At the end of each clinical rotation with a SLP, a formal review of the SLP must be completed and discussed with the student. This includes:
- Reassessing/adding competencies at risk, identifying competencies successfully completed, and those competencies that the student had limited opportunity to demonstrate. (SLP Part B: Competencies at Risk)
- Document a review of contract (SLP Part A: Review of Contract). Please add brief comments on the students’ progress and any further actions required in the table. Supporting documentation should be included in the student’s final clinical evaluation.
- Meet with the student to discuss the review of contract. A copy of the current SLP will be sent to the student’s PAWS email account (cc clinical instructor/FRP, Course Coordinator and Advisor). The student must reply stating they have read and understood the SLP prior to returning to the clinical setting (if applicable). By replying the student acknowledges they have received a copy of the SLP and have had an opportunity to discuss it with their instructor/course coordinator.
When a student is on a SLP that will be carried forward to the next clinical rotation the Academic Advisor will email the student the SLP, and copy the Course Coordinator who will notify the clinical instructor/FRP. The student is ultimately responsible for informing and sharing their SLP with the next Clinical Instructor or FRP. This is necessary to enhance student learning opportunities and success, and to ensure patient safety.
Performance issues may be resolved at this juncture or may move to Process #3 or directly to Section B.
3. Student remains at minimal pass with persistent performance issues while on SLP:A formal meeting with the student, Course Coordinator and/or Clinical Instructor/FRP will be held to discuss performance issue and the student’s ability to meet the course objectives in the remaining clinical time. Academic Advisors, student support persons and the Associate/Assistant Dean may be present at this meeting. Issues and additional success strategies will be reviewed with the student and included in the SLP. A follow up email with written documentation of the discussion will be sent to the student’s PAWS email account. The student must reply stating they have read and understood the performance issues prior to returning to the clinical setting (if eligible).
4. Student receives minimal pass on final evaluation:In the event a student receives a minimal pass on the final evaluation, a SLP must be carried forward to the next clinical course. The minimal pass will be tracked by the Academic Advisor as per the College of Nursing Grade Assignment Policy:
A minimal pass grade of 50 - 59, as per the Literal Descriptors, in clinical is only allowed once throughout the program. If a student obtains a minimal pass a second time, the student will receive an N (No credit) grade and will be required to repeat the course and receive a minimum of a satisfactory grade of 60 - 69, as per the Literal Descriptors, in that clinical course and in all subsequent clinical courses.
When a student is on a SLP that will be carried forward to the next clinical rotation the Academic Advisor will email the student the SLP, and copy the Course Coordinator who will notify the clinical instructor/FRP. The student is ultimately responsible for informing and sharing their SLP with the next Clinical Instructor or FRP. This is necessary to enhance student learning opportunities and success, and to ensure patient safety.
Section B: Processes to be used when there is unsafe or potentially unsafe performance in the clinical/lab setting resulting in failure in, or withdrawal in lieu of failure from a clinical/lab course.
1. Failure in a clinical course:
Documentation should include clear rationale for the failure or withdrawal in lieu of failure. Including:
-
-
- Description of performance concerns or any untoward incidents during the clinical experience
- Documentation of any meetings that were held with the student that outline the clinical difficulties being experienced, the possible consequences of no improvement in performance, plans for improving and evidence the student has been informed and has identified a plan for improvement
- Student performance should be discussed in relation to the literal descriptors and the clinical evaluation tool.
- Student will receive a clinical evaluation
-
At the time of the assignment of a failing grade or withdrawal in lieu of failure:
-
-
- Associate/Assistant Dean and Academic Advisor will be notified
- Clinical Instructor/FRP and/or Course Coordinator will meet with the student to discuss the failure or withdrawal in lieu of failure. Academic Advisors, student support persons and the Associate/Assistant Dean may be present at this meeting. The following will be discussed:
- evidence leading to the assignment of a failing grade or decision to withdraw in lieu of failure
- exploration of possible reasons
- strategies the program may initiate in order to support the student if s/he repeats the course
- Document the meeting and provide copies to all parties by email. Inform the student of the right to appeal a failing grade and the appeal process
- If not already in place, a SLP will be initiated, in consultation with the course coordinator, per Process A #3 above
- Student will be advised to meet with an Academic Advisor:
- a change in program will be created if the student is eligible
- strategies to assist the student to be successful will be discussed and documented on the change in program.
- student will sign and receive a copy of the change in program which will be placed in the student's file and a copy will be sent to the Clinical Coordinators.
- change in programs will be reviewed by the Associate/Assistant Dean as necessary
-
Download Student Learning Plan
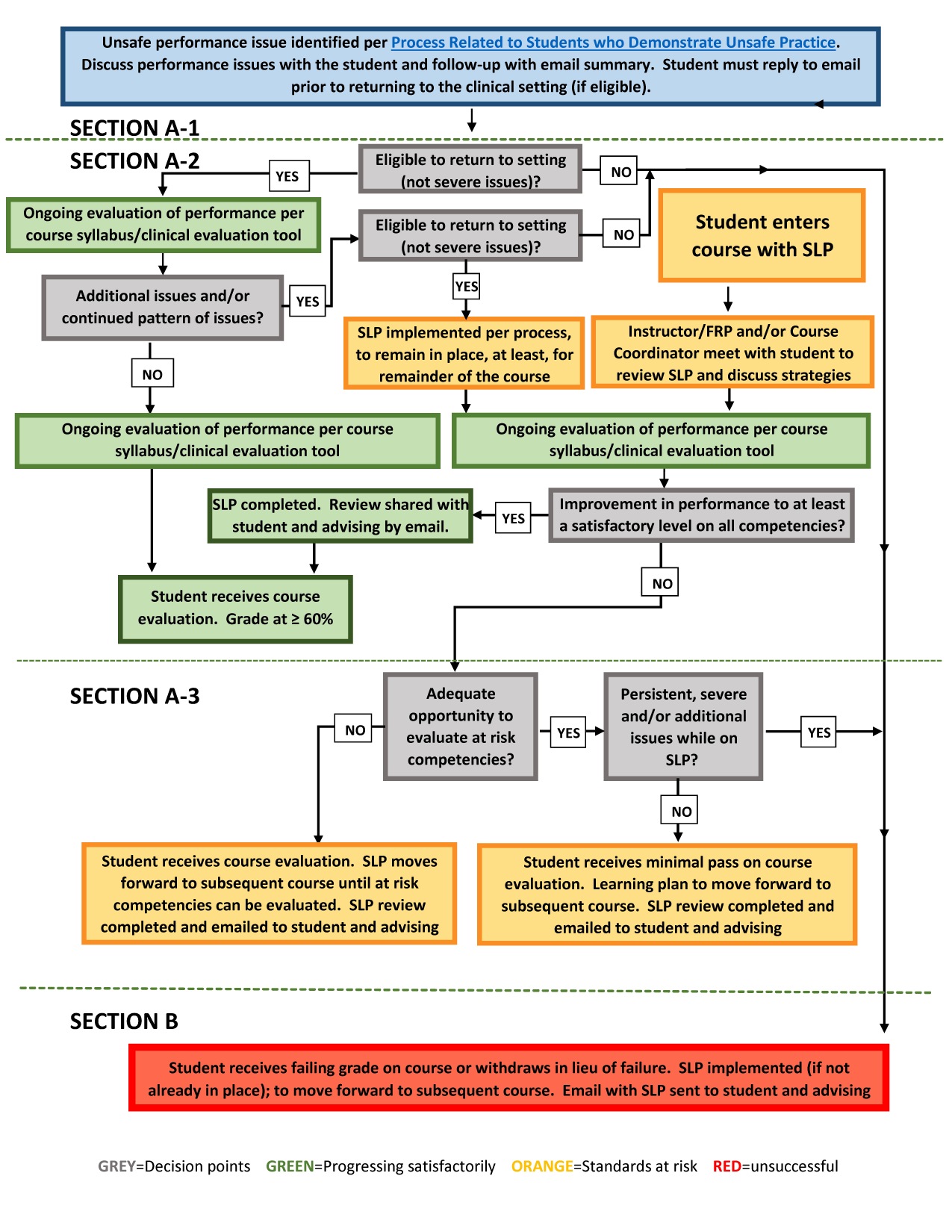
SLP Process PDF
SLP Flowchart PDF
SLP Follow Up Email Template
References
Canadian Association of Schools of Nursing and Canadian Patient Safety Institute (2018). Learning Outcomes for Patient Safety in Undergraduate Schools of Nursing Curricula. Ottawa, ON: Author.
Canadian Nurses Association (2004). Nurses and Patient Safety: A discussion paper. Ottawa, ON: Author.
Killam, L. A., Luhanga, F., & Bakker, D. (2011). Characteristics of unsafe undergraduate nursing students in clinical practice: An integrative literature review. Journal of Nursing Education, 50(8), 437-446.
Scanlan, J., Care, W., & Gessler, S. (2001). Dealing with the unsafe student in clinical practice. Nurse Educator, 26(1), 23.
Purpose
- To promote a professional style of dress appropriate for the delivery of professional nursing care.
- To promote communication by clearly identifying name, year in program for students or faculty role.
- To promote infection prevention and control.
- To comply with safety guidelines and pertinent legislation.
Policy
Students who are not following the principles of this policy may be asked to leave the clinical setting. In this case, the time away will be considered under the Attendance Policy.
Considerations may be made for individual dress that is specific to cultural or religious beliefs.
Clothing
- Wear a College of Nursing standard uniform for all clinical settings unless otherwise specified. Garments worn under the uniform top must not be colored or long sleeved. Uniforms must be clean, in good repair and appropriate in fit. Pants should be hemmed above the heel line. Uniform skirts should be at knee level or below. Uniforms should fully cover undergarments.
- Uniforms are not to be worn to and from the clinical setting. Uniforms should be changed/cleaned daily. If a student’s uniform is contaminated with blood or bodily fluid during a shift the student must change. The RHA/SCA will provide decontamination services if appropriate and provide the student with an alternative uniform for the remainder of the shift.
- The College of Nursing uniform consists of a white top and a green bottom or matching green top and bottom with the College of Nursing logo embroidered directly on the front upper left of the top.
- Where appropriate and necessary, students will follow the protocols of individual departments, units or services that have specific dress code requirements.
- In settings where the standard uniform is not worn (e.g., Community), students should demonstrate good judgment in selecting appropriate clothing to display a professional image while following the specific dress requirements of the agency. Clothing should not be low cut at the neck or tight across the chest and hips. Ensure that there is no exposure of the chest, midriff, lower back, or shoulders. Undergarments should not be visible at any time. Avoid casual clothing such as sweatshirts, yoga pants, jeans.
- Gowns/protective wear provided on a unit shall not be worn off the unit or for any other purpose than it was intended for.
Shoes
- Shoes must have closed toes and closed heel with a non-slip, non-marking sole and low heel.
- Must be clean and in good repair
- Must be easily wipe-able in the event of contamination.
- Footwear used in the clinical setting is not to be worn outside of the clinical setting.
Hair
- Must be clean and well groomed. Long hair must be tied up and away from the face.
- Beards and mustaches must be clean and well-groomed.
Fingernails
- Short and clean
- No nail polish
- No artificial/gel nails/nail extensions
Jewelry
- Plain, flat, smooth rings may be worn. Cannot wear rings with exposed stones.
- No bracelets unless a medical ID bracelet (must be taken off during hand washing)
- Watches can be worn high on the arm or taken off during hand washing. Must be cleaned after each shift.
- Can include necklaces if worn inside of clothing.
- Small stud like earrings may be worn.
Piercings
- Only very small, securely fastened stud like jewelry may be worn in facial or other visible body piercings, including tongue piercings.
- Shall not include piercings on the hand or wrist.
- Those piercings that are unhealed or infected will be covered and contained before commencing duty.
Tattoos
- Tattoos shall be covered if deemed inappropriate by the clinical instructor, unit, or service manager during clinical placements (if doing so does not interfere with proper infection control techniques such as hand hygiene).
- Tattoos that are unhealed or infected will be covered and contained before commencing patient care.
Cosmetics
- Perfume, cologne, and other scented body products shall not be worn.
- Other cosmetics should be worn in moderation. Use good judgment in wearing appropriate quantity of makeup.
Personal Hygiene
- Students should practice good personal hygiene, including control of body odor and cleanliness.
Stethoscope
- When not being used, stethoscopes must be kept in your pocket
- Stethoscopes should be cleaned between each patient.
Photo/Role Identification
- College of Nursing photo ID badge must be worn and visible at all times. ID badge is to be worn at chest level.
Purpose
To clarify the expectations surrounding students attending professional conferences.
Policy
- Active participation in professional student conferences is important to advancing the nursing profession, strengthening collaboration and communication and building leadership skills. Nursing students should be encouraged to attend local, provincial and national student conferences, when appropriate and relevant. Conference attendance should be prioritized with course and clinical workload expectations. It is the student’s responsibility to ensure that they can continue to meet course and program objectives and requirements.
- Students interested in attending conferences must currently be in good academic standing, have a cumulative weighted nursing average of 70% in the academic year prior to requesting approval for conference attendance. Students missing clinical/lab must be clinically proficient (e.g. have no active student learning plan).
- Students interested in attending conferences must submit the signed Application for Student Conference Attendance Request form to their academic advisor no later than 2 months prior to the start date of the conference.
- Students attending a conference must sign the Application for Student Conference Attendance Request form acknowledging that they understand the attendance policy and that if the student misses more than 10% of clinical/lab experiences in a course, he/she may be unable to meet the course requirements, and thus may not receive credit for the course. This completed form is to be returned to the student’s academic advisor.
- The student must send the completed Conference Attendance Request form, when verified by an academic advisor, to the course lead for all the classes they will be missing.
- It is up to the course lead to determine if the conference can be used in lieu of clinical time. Students may only attend one conference in lieu of clinical time per academic year. Subsequent missed time due to conference attendance will be considered missed clinical time.
- Student are responsible for notifying all instructors of their planned absence.
- Students who attend a conference without submitting the Application for Student Conference Attendance Request form and notifying the instructor and/or academic advisor on time, will be considered absent from clinical/lab and this will count towards the 10% missed clinical time.
Purpose
To define the maximum timeframe for program completion.
Policy
- For students admitted to the BSN program - all required courses must be completed within six years of admission to nursing.
- For students admitted to the Post-Degree BSN option - all required courses must be completed within three years of admission.
- Extensions may be granted under certain circumstances for those individuals who are making steady progress towards successful completion of the program. Such cases are reviewed upon receiving a written request from the student.
Purpose
To delineate the process for students who attempt clinical nursing courses multiple times.
Policy
- A minimal pass grade of 50 - 59, as per the Literal Descriptors, in a clinical course is only allowed once throughout the program (as defined in the processes related to students who demonstrate unsafe practices policy). If a student obtains a minimal pass a second time, the student will receive an N (No credit) grade and will be required to repeat the course and receive a minimum of a satisfactory grade of 60 - 69, as per the Literal Descriptors, in that clinical course and in all subsequent clinical courses (Please refer to CoN Repeating a Course Policy).
- A failing grade or a withdrawal in a clinical course is only allowed once throughout the program. If a student obtains a failing grade or withdraws a second time in another clinical course (as defined in the processes related to students who demonstrate unsafe practices policy), the student will be required to discontinue from the College of Nursing. If a student must withdraw from any subsequent clinical course due to exceptional circumstances beyond their control they may request to continue in the program. See process in # 4 below.
- Undergraduate students in the College of Nursing may attempt the same nursing clinical course twice. Withdrawals from a nursing clinical course for academic reasons will be considered an attempt.
- In exceptional circumstances, permission may be granted by the college for a third and final attempt Students wishing to attempt a course for the third time must submit a written request to the site-specific Associate/Assistant Dean within 30 days of their failure or withdrawal from the course.
- Students who are granted a third attempt at a clinical nursing course may not progress into other clinical courses until they have successfully passed their third attempt.
- Clinical courses being attempted for a third time may require mandatory remedial course work. A student who fails or withdraws from any clinical course for a third time will be required to discontinue study in the College of Nursing and will be advised of this in writing.
- Students repeating any courses must meet with an academic advisor to complete a change of planned progression in the program.
Definitions:
- Course Withdrawal – Withdrawal from a course before the deadline for registration changes, (which is the deadline to add/drop classes) will not be considered an attempt at the course and will not be tracked as an attempt.
- Minimal Pass in Clinical Practice Component – a mark of 50-59% in accordance with the clinical evaluation tool.
- Failure in Clinical Practice Component – a mark of <50% in accordance with the clinical evaluation tool.
Purpose
To outline the process for promotion through the BSN and PDBSN programs in the College of Nursing, and the recognition of student academic achievement.
Policy
- Students are required to maintain a cumulative weighted academic average of 60%. The following information guides the determination of continuation within the program.
- A cumulative weighted average below 60% - student is required to discontinue.
- A cumulative weighted average between 60 – 65% - student will be required to repeat any courses with marks below 55% and will be recommended to repeat any course with a grade between 55 - 59%.
- Students with a cumulative weighted average below 65% will be sent a letter encouraging contact with an academic advisor to discuss academic supports.
- As per the Grade Assignment Policy - A minimal pass grade of 50 - 59, as per the Literal Descriptors, in clinical is only allowed once throughout the program. If a student obtains a minimal pass a second time, the student will receive an N (No credit) grade and will be required to repeat the course and receive a minimum of a satisfactory grade of 60 - 69, as per the Literal Descriptors, in that clinical course and in all subsequent clinical courses.
- Students may be required to discontinue their studies at any point in their nursing program for reasons other than academic, if it is considered in the best interest of the profession or if continuation in the program is deemed to be unsafe to themselves or others.
- Dean’s Honor Roll
Students with a cumulative weighted average in the top 10% in years two and three of the program will receive a congratulatory letter recognizing placement on the Dean’s honor roll. - Graduation
To graduate, students must have passed all required courses in the program with a minimum cumulative weighted average of 60%. - Convocation
At convocation, students with cumulative weighted averages in the top 20% of the graduating class will be awarded distinction or great distinction.- Students with cumulative averages in the top 5% of the graduating class will be awarded great distinction.
- Students with the next cumulative averages in the top 15% of the graduating class will be awarded distinction.
Purpose:
To delineate the process of repeating a course.
Policy:
Section 1. Applies to all students
- Students repeating any courses must meet with an academic advisor to complete a change of planned progression in the program.
- If a student achieves a grade of 60% or higher, a course can be repeated only with permission of the Associate/Assistant Dean at the appropriate site.
- If a course is repeated, the repeated course must be passed, and the grade of the repeated course will be used in calculating the weighted average.
- Undergraduate students in the College of Nursing may attempt a course twice. Withdrawals from a course after the add/drop deadline will be considered an attempt.
- A student who fails or withdraws from a course for a second time will be required to discontinue study in the College of Nursing and will be advised of this in writing.
- In exceptional circumstances, permission may be granted by the College for a third and final attempt in a course. Students wishing to attempt a course for the third time must submit a written request to the site specific Associate/Assistant Dean within 30 days of their failure or withdrawal from the course.
- Students who have had a delay in their program progression may be required to repeat courses, as determined by the associate/ assistant deans.
Section 2. Applies to students admitted prior to September 2021
- Undergraduate students in the College of Nursing may attempt a clinical course twice. Withdrawals from a clinical course after the add/drop deadline will be considered an attempt.
- A student who fails or withdraws from a clinical course for a second time will be required to discontinue study in the College of Nursing and will be advised of this in writing.
- In exceptional circumstances, permission may be granted by the college for a third and final attempt in a clinical course. Students wishing to attempt a clinical course for the third time must submit a written request to the site specific Associate/Assistant Dean within 30 days of their failure or withdrawal from the course. Clinical courses being attempted for a third time may require mandatory remedial course work.
- Students who are granted a third attempt at a clinical nursing course may not progress into other clinical courses until they have successfully passed their third attempt.
- A student who fails or withdraws from a course for a third time will be required to discontinue study in the College of Nursing and will be advised of this in writing.
Purpose
To establish guidelines for respiratory mask fit testing of students consistent with the most current Occupational Health and Safety Regulations and the Canadian Standards Act prior to and during clinical placements. Proper respiratory mask fitting helps to protect students from respiratory infection when providing care or service to clients with acute respiratory infections.
Policy
All nursing students will be fitted with an N95 respiratory mask and educated on its use when required during the program.
- Arrangements will be made by the College of Nursing for each student to attend a session to be fitted for the most appropriate type and size of respiratory mask.
- Students who fail to attend their scheduled session must make their own arrangements for fit testing.
- Students who are unable to comply with this requirement may be at risk of not being able to complete required components of the program.
- Students are required to have information regarding their respiratory mask type and size with them while in the clinical setting. Students must carry proof of fit testing results on their person at all times during the placement experience.
- If a student cannot be fitted for a respirator then they cannot enter any clinical placement area requiring a respirator.
- Notify the appropriate person in the RHA/SCA and their education program if they are exempt from fit testing.
- In accordance with the Canadian Standards Act, students are required to be refitted at least every two years while in the program or earlier if they have changes to face shape, size or features.
Purpose
To delineate the process for the writing of supplemental examinations.
Policy
- To be eligible to apply for a supplemental final examination, where the final exam is NOT an essential component, a student must have obtained a final mark of 40-49% in the course and have failed the final exam. In addition, the student must have a weighted overall average and weighted nursing average of at least 60% for the academic term.
- To be eligible to apply for a supplemental final examination, where the final exam IS an essential component, a student must have obtained a final mark of at least 40% in the course and have failed the final exam. In addition, the student must have a weighted overall average and weighted nursing average of at least 60% for the academic term.
- Supplemental examinations must be applied for within three (3) weeks of the end of the examination period.*
- No supplemental examination will be granted for courses that do not have a final examination.
- University level policies related to supplemental examinations are outlined in the University Council Regulations on Examinations
- Supplemental examinations will not be granted for clinical experience.
*NOTE: Applications for the supplemental examination for the Post Degree BSN courses have a shorter timeframe. Please contact an Academic Advisor at the College of Nursing.
Purpose
To ensure transferring, lifting and repositioning (TLR) requirements are clear and consistent for all undergraduate students.
To ensure the safety of students, practitioners and patients during transferring, lifting and repositioning activities during student clinical placements.
Policy
- All students must receive and maintain current TLR certification prior to the first clinical placement and throughout the program. Re-certification is required every three years.
- Students must provide evidence of current TLR certification prior to the start of the first clinical experience.
- Students failing to provide evidence of current TLR certification will be excluded from clinical practice.
Purpose
To outline the guidelines for allocating the relevant weight for final examinations and the clinical component in courses.
Policy
- Final examinations shall be no more than 50% and no less than 30% of the final grade, unless approved by the Undergraduate Education Committee. No supplemental examination will be granted in a course that has not had a final examination.
- In nursing courses that have a clinical component, the portion allocated to the practice component shall be not less than 30% and no more than 50%, unless otherwise approved by the Undergraduate Education Committee.
Purpose
To establish consistent recommendations for WHMIS (Workplace Hazardous Materials Information System) training for College of Nursing students.
Policy
Students participating in a clinical placement must successfully complete the most current WHMIS training within the year previous to their first clinical placement, and provide proof of completion to the College of Nursing prior to clinical placement.
- Students are required to complete the necessary online training through Workplace Safety and Environmental Protection, University of Saskatchewan. No other WHMIS certificate will be accepted.
- Students must retake the online WHMIS training through Workplace Safety and Environmental Protection, University of Saskatchewan every three years as per University of Saskatchewan safety training requirements.
During clinical placements and in consultation with the on-site faculty and/or site supervisor students must:
- Select and use appropriate personal protective equipment when working with controlled produc Follow all safe work place practices when working with controlled products/hazardous materials.
- Understand how to read and interpret supplier labels and hazard symbols.
- Know where the MSDS information (binder or on-line) is located and how to interpret/understand them.
Report to on-site faculty and site supervisor any unusual or unsafe situations within the placement department.
Purpose
To ensure that all nursing students are eligible for Workers’ Compensation Board (WCB) benefits if they sustain an injury during the course of a work-based learning assignment (clinical placement).
Policy
- All nursing students will complete the WCB Agreement Schedule "C" Work-Integrated Learning Consents and Waiver of Liability, at the start of the program, prior to the first clinical placement. This one form will apply to all clinical placements.
Note: Coverage is not applicable or available for any placement or portion of a placement that takes place outside of Saskatchewan or on a First Nation. - WCB forms must be signed by the student, witnessed, and returned to the College of Nursing.
- Original signed copies of WCB forms will be retained by the College of Nursing for a minimum of two years from the completion of the program to correspond with provincial statutes.
- In the event of an injury sustained during a clinical placement:
- The student must notify the Course Coordinator
- The Course coordinator notifies the clinical coordinator
- The student must report the injury to the WCB using the Workers Initial Report of Injury (W1)
- The clinical coordinator must report the injury to the WCB using the Employer’s Report of Injury (E1) form.
- Reporting by the student and Clinical coordinator must occur within five days of the incident.
- Form Submission:
- W1 and E1 forms must be submitted by one of the following methods:
- Online: https://myaccount.wcbsask.com/online-services/report-an-injury
- Email: forms@wcbsask.com (please send either a picture (JPEG) or a PDF document)
- W1 and E1 forms must be submitted by one of the following methods:
- Annual Reporting:
- The College of Nursing must provide an annual report to the Ministry of Advanced Education, which confirms:
- the total number of participating students in WCB benefits for the current academic year;
- the number of work-based learning assignments (clinical placements) undertaken in the current academic year;
- that each participating student has signed a WCB Agreement Schedule "C" Work-Integrated Learning Consents and Waiver of Liability.
- The College of Nursing must provide an annual report to the Ministry of Advanced Education, which confirms:

